Articles
The Hidden Ectopic
Author: Admin
Case Report46-year-old lady, nulliparous, was a known case of severe endometriosis with adenomyosis. She had undergone 3 laparoscopic surgeries, first in 1993 for bilateral endometriotic cysts, and the last one in 2013, which showed dense bowel adhesions to the uterus with both adnexa completely covered with bowel adhesions.
She had a hydrosalpinx for which she underwent right salpingectomy during the last laparoscopy.
Husband was diagnosed with non obstructive azoospermia with elevated FSH levels.
She underwent IVF in October 2015, during which 2 embryos were transferred. Her beta hcg on day 14 was 1810. When repeated after 4 days, the value was 8025.
An ultrasound was done which revealed no intrauterine or extrauterine sac. Patient was followed up with beta hcg levels, after 2 days, which became 24813. Patient was asymptomatic, and value repeated after 2 days was 28222. Ultrasound repeated again, showed no intra uterine or extrauterine sac, and an endometrium of 9mm in thickness.
Since value was extremely high, and as no intrauterine pregnancy was localized on ultrasound, patient and bystanders were counseled and taken up for operative laparoscopy.
At laparoscopy, the bowel was seen densely adherent to both adnexa, making it difficult to visualize the adnexa. Bowel (rectosigmoid) was adherent to the posterior surface as well as fundus of the uterus.
The bowel adhesions near the left adnexa were released by sharp dissection. Bowel adhesiolysis could be only done partially since there was a high risk of bowel injury. At one point, tissue resembling chorionic tissue was seen projecting out from a structure resembling the fallopian tube. Tube could not be identified separately. Chorionic tissue was taken for histopathological examination. Bleeding points were identified from the suspected base of the tube, which was coagulated using microbipolar cautery. Since the vital structures like ureter and iliac vessels were extremely close to the lateral wall, further coagulation of the bleeding points could not be done. Drain was inserted and patient was followed up with serial βhcg. 4 days after the surgery, decreased to 3110 mIU/ml. The following week the value was 526 mIU/ml. She was followed up with expectant management with serial weekly monitoring of βhcg. The value reached negligible limits 5 weeks after surgery.


Image1: Right adnexa adherent to bowel.
Image2: Left adnexa completely covered
with dense bowel adhesions
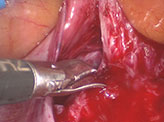

Image3: Bowel adhesions partially released.
Image4:Products of conception retrieved through left lateral port.
An ectopic pregnancy is the implantation of the fertilized ovum outside the uterine cavity. The incidence of ectopic is around 1-3%. Though there are no major identifiable risk factors, a common factor for ectopic pregnancy is prior damage to fallopian tube.
Useful ultrasonographic findings in the diagnosis of ectopic pregnancy
- Absence of intrauterine pregnancy (IUP)
- Positive identification of an ectopic pregnancy mass: inhomogenous mass, empty adnexal gestation sac or adnexal sac containing yolk sac or fetal pole
- Free fluid (i.e. blood): suggestive of ectopic pregnancy in the absence of IUP, but not diagnostic (small amount may be physiological (2)
In cases where an ectopic pregnancy is suspected and ultrasound is inconclusive, a diagnostic laparoscopy may be required. This is believed by many to be the ‘gold standard’ investigation in ectopic pregnancy. Indeed reluctance or delay in performing a diagnostic laparoscopy has been highlighted as a factor in fatal cases (1)
However, some small ectopic pregnancies may be missed at the time of laparoscopy or laparotomy. An alternative to diagnostic laparoscopy may involve a repeat ultrasound examination, particularly when β-hCG concentrations are close to 1500 IU/l. Other strategies include alternative diagnostic tests, such as serum progesterone or an endometrial biopsy, or empirical medical treatment as the patient may well have an ectopic pregnancy. If β-hCG concentrations are falling but an ectopic has not been excluded, consideration should be given to performing serial β-hCG measurements until levels become undetectable, as rupture can still occur.
In selected cases of PUL, an endometrial biopsy may be taken and analysed for the presence or absence of chorionic villi. Their absence in the presence of a static β-hCG is suggestive of an ectopic pregnancy. A dilatation and curettage may be useful when performed in association with a ‘negative’ diagnostic laparoscopy for a suspected ectopic pregnancy. The clinician should be certain that the pregnancy, if intrauterine, is non-viable and appropriate consent obtained, as this procedure could potentially interrupt a continuing pregnancy
References1. Robson SJ, O’Shea RT. Undiagnosed ectopic pregnancy: a retrospective analysis of 31 ‘missed’ ectopic pregnancies at a teaching hospital. Aust N Z J Obstet Gynaecol. 1996;36:182–185
2. Barnhart KT, Sammel MD, Rinaudo PF, et al. Symptomatic patients with an early viable intrauterine pregnancy: HCG curves redefined. Obstet Gynecol. 2004;104:50–55

